Endometriosis
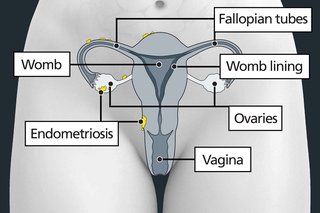
Endometriosis is where cells similar to those in the lining of the womb (uterus) grow in other parts of the body. It can have a big impact on your life, but there are treatments that can help.
 Credit:
Credit:
Multimedia Team - nhs.uk
Symptoms of endometriosis
Endometriosis usually grows in areas around the womb, such as the ovaries and fallopian tubes. It can also affect organs such as the bladder and bowel.
Symptoms happen when patches of endometriosis break down and bleed during your period but cannot leave your body.
You might have some symptoms during your period, such as:
- severe period pain, that stops you from doing your normal activities
- heavy periods, where you need to change your pads or tampons every 1 to 2 hours, or you may bleed through to your clothes.
- pain when you poo or pee
You can have other symptoms at any time in your menstrual cycle, such as:
- pain in your lower tummy and back (pelvic area)
- pain during or after sex
- extreme tiredness (fatigue)
You may also have difficulty getting pregnant and have low mood or anxiety.
Endometriosis is commonly diagnosed in women and girls, from when their periods start (puberty) through to menopause. It can affect anyone who has periods.
Tests for endometriosis
It can take a long time to diagnose endometriosis. You might need several different tests to find out if you have it.
This is because endometriosis symptoms can be similar to other conditions, such as:
What happens at your GP appointment
A GP will ask about your symptoms and may ask to do:
- a physical examination (including an internal vaginal exam) – to check your tummy (abdomen) and your pelvic area
- blood tests
Give your GP as much information about your symptoms as you can.
If they think you might have endometriosis, your GP may:
- refer you to a specialist called a gynaecologist for further tests
- offer medicines to help relieve your symptoms
Further tests
Further tests for endometriosis include:
- an ultrasound scan – this may be an internal vaginal scan
- a procedure called a laparoscopy (where a camera is passed through a small cut in your tummy) – this can confirm if you have endometriosis
It may be possible for doctors to remove any areas of endometriosis during your laparoscopy.
Treatments for endometriosis
It’s not known what causes endometriosis and there are currently no treatments that can cure it. But treatment can help manage symptoms such as pain.
Your doctor will talk to you about the risks and possible side effects of each treatment.
If treatment is not working or your symptoms are very severe, you may be referred to a specialist endometriosis service.
Medicines for endometriosis
Medicines are often the first treatment for endometriosis. They include:
- painkillers, such as paracetamol and ibuprofen
- hormones, such as the combined contraceptive pill – these can help ease pain
Surgery for endometriosis
If other treatments are not working or you have lots of endometriosis, you may be offered surgery. Surgery is also an option if endometriosis is affecting your ability to have children.
You can have surgery to:
- remove areas of endometriosis or fluid-filled sacs (ovarian cysts) caused by endometriosis
- remove your womb (hysterectomy) or ovaries (oophorectomy)
- remove part of your bladder or bowel, if endometriosis is affecting these
You may need to have more surgeries if your symptoms come back after your first surgery, or if surgery causes scarring that makes your organs to stick together (adhesions).
Support for living with endometriosis
Treatment and support are also available for other problems caused by endometriosis.
Support you might need includes:
- advice on ways to manage long-term pain and extreme tiredness (fatigue)
- referral to a fertility specialist if you have difficulty getting pregnant
- mental health support if you have low mood or anxiety
Reasonable Adjustments for Women with Endometriosis
Endometriosis can significantly affect physical, emotional, and work-related functioning. Occupational health will be able to assist you further but here are tailored adjustments to help manage the condition in the workplace:
1. Flexible Working Arrangements
- Flexible Hours: Allow later start times or a phased return if mornings are particularly difficult due to pain or fatigue.
- Work from Home: Permit remote working during flare-ups to avoid travel-related discomfort.
2. Adjusted Workload
- Task Prioritisation: Redistribute non-essential tasks during difficult periods.
- Reduced Hours: Consider temporary reductions in working hours during particularly severe phases.
3. Time Off for Medical Needs
- Medical Appointments: Provide flexibility for attending doctor visits, physiotherapy, or treatments.
- Recovery Periods: Allow additional sick leave or unpaid leave for recovery after surgeries or severe flare-ups.
4. Physical Comfort
- Ergonomic Adjustments: Provide adjustable chairs, standing desks, or supportive seating to improve comfort during work hours.
- Access to Rest Areas: Allow use of a private space for resting or managing symptoms during the workday.
- Accessible Facilities: Ensure easy access to clean and private restrooms, as frequent use may be necessary.
5. Emotional Support
- Access psychology/ counselling: Highlight the services to your staff to assist managing stress or mental health impacts.
- Regular Check-Ins: Schedule supportive conversations with managers to review well-being and workload.
6. Work Environment Modifications
- Reduced Standing: Limit tasks that require prolonged standing or walking.
- Supportive Equipment: Provide lightweight tools or carts to reduce physical strain when handling equipment or documents.
7. Planning for Fluctuations
- Contingency Planning: Create a plan to manage work during unexpected flare-ups, such as assigning a backup for critical tasks.
- Advance Notice: Encourage employees to notify their manager of upcoming periods of anticipated difficulty (e.g., around menstruation or surgery).
8. Training and Awareness
- Managers to increase understanding: We encourage managers to have an open conversation about the impact that endometriosis has on their colleague this will foster understanding and ensure sensitivity in workplace interactions.
- Open Culture: Promote an inclusive environment where employees feel comfortable discussing their health needs.
Utilise the Wellbeing at Work Action plan to structure your wellbeing conversation and ascertain what support is required.