In a UK-first, a grandad of 19 who fell critically ill with a rare blood disorder has received a new life-saving drug as part of a clinical trial at Liverpool University Hospitals NHS Foundation Trust (LUHFT).
David Cope, 67, from Thameside in Manchester, was diagnosed earlier this year with Thrombotic thrombocytopenic purpura (TTP), a rare blood disorder causing blood to clot in small blood vessels throughout the body, stopping blood flow to major organs.
He became the first patient in the UK to be given an Intravenous (IV) treatment for TTP, as part of an international clinical trial. This is less invasive than the standard treatment for TTP, which requires several plasma exchanges, round-the-clock care and can see patients put into an induced coma.
David lives an active lifestyle and retired in January this year after a career as an electrician. As a proud dad of six, and grandad of nineteen, David splits his time between his Thameside home and his caravan in Prestatyn, Wales.
Earlier this year, David noticed he was unable to keep up with his usual daily activities, becoming tired quickly as well as experiencing pains in his chest and head.
David said: “I felt run down for a few weeks and my wife suggested I go get checked out but didn’t think much of it."
“The day before I was admitted to hospital, we were taking care of our grandchildren when I started to feel really unwell and my eyesight began to go. We decided as a family it was right for me to go to A&E, and it was all systems go from there.”
After David presented at his local hospital with many symptoms of TTP he underwent tests and scans confirming the diagnosis. He was transported to the Intensive Care Unit at the Royal Liverpool University Hospital, which is run by LUHFT and has one of the largest TTP Specialist Centres in the country, looking after around 100 TTP patients from across the region.
Patients with TTP experience symptoms including fever, fatigue, headaches, confusion, rashes, bruises and stroke-like symptoms. The condition is fatal without treatment and can have drastic effects on everyday life.
The standard treatment for TTP is an intensive plasma exchange procedure which is often required for around a week lasting 4-5 hours daily. Plasma is the part of the blood which carries red and white blood cells including antibodies to help fight infection.
Plasma exchange removes the existing plasma from the patient with TTP and replaces it with new plasma to help regulate their condition.
Many patients require round the clock care from doctors and some are placed in an induced coma to protect their organs from the stress of the condition.
LUHFT is the only site in the UK to offer an international clinical research trial, which reduces the number of exchanges needed, replacing it with an Intravenous treatment that can be given through a small needle in the arm.
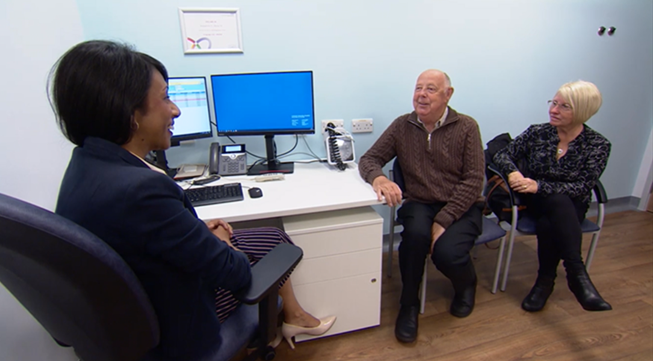
David was admitted to the care of Dr Tina Dutt, Consultant Haematologist, TTP Specialist Centre and Haematology Research Lead at LUHFT.
Dr Dutt discussed with David and his family that this clinical trial opportunity could avoid extended treatment with plasma exchange, whilst also treating this rare disease.
Dr Dutt said: “When Mr Cope arrived on site, he was very unwell and we knew we needed to act quickly. He required around-the-clock care and was at one point was placed on a life support machine due to a deterioration in his neurological state.
“I discussed the trial opportunity with David and his family when they arrived, explaining that whatever they decided to do, we would do our best to effectively treat and control the condition.
“So far, we have seen encouraging results with this new treatment and David’s condition has continued to improve. Despite presenting with kidney failure, cardiac and neurological problems, David only required two days of plasma exchange and was ready for discharge from ITU after 4 days.
“This disease and the current standard of care treatment options can take a huge toll on the patient. We are committed to delivering research opportunities that can potentially improve patient care and outcomes. Mr Cope and his family have engaged with the whole team from the time of arrival, having a positive spirit throughout their journey.
“A rare disease like David’s is not rare for a patient who is living with it, so it’s important that we drive forward research in these areas.”
David’s wife Julie was by his side throughout the process.
Julie said: “The experience was terrifying, we spent days not knowing what was wrong or what was going to happen to David. After speaking to David, Dr Dutt and her team spoke to my son and I, to ask us how we felt about David taking part in a clinical trial. This was amazing, we felt like we were a really important part of the care David was going to receive.”
Now back home with his family, David is feeling much better with his blood levels continuing to stabilise. TTP is a life-long condition however, through research and new treatments, clinicians hope to find ways to reduce the severity of treatment and the number of flare-ups a patient will have in their lifetime.
David is currently undergoing treatment and monitoring by teams at LUHFT and is looking forward to getting back to his North-Wales caravan where he plans on spending the summer months with his wife.

David said: “From not knowing what TTP was a few weeks ago, to now surviving and living with it, I can’t thank the team at Liverpool enough for all they did.
“It’s like a family there. I was scared to be facing such an unknown disease, but the team made me feel like I had known them all my life.”
If you would like more information on how you could get involved in research at LUHFT, please click here.